Between Saturdays: Why Salt Still Raises Your Blood Pressure… Even When You Barely Use It
The science of why mineral balance matters more than just cutting salt — feel lighter & more balanced fast
For years, the public message around blood pressure has been simple: eat less salt. The science, however, has always been more layered. Sodium doesn’t act in isolation. It moves through a tightly regulated system involving potassium, magnesium, kidney function, and vascular tone. This week’s studies show that when sodium is reduced inside the right mineral environment, the body responds very differently.
Caught My Eye…
Sodium reduction works best inside a potassium and magnesium rich diet
The DASH–Sodium Trial remains one of the most informative feeding studies on blood pressure. Adults were assigned either a typical control diet or the DASH diet, then cycled through high, intermediate, and low sodium levels for 30 days each.
What mattered most wasn’t sodium alone. The largest blood pressure reductions occurred when low sodium was combined with the DASH diet, which intentionally raises potassium, magnesium, calcium, fiber, and protein.
Compared with a high-sodium control diet, low-sodium DASH lowered systolic blood pressure by about 7 mmHg in people without hypertension and more than 11 mmHg in those with hypertension.
The takeaway is subtle but important: sodium’s effect depends on the mineral context surrounding it. Potassium and magnesium alter vascular tone and kidney handling of sodium, amplifying the benefit of sodium reduction.
A simple mineral swap lowered blood pressure without changing the whole diet
A randomized trial published in the BMJ tested a practical idea in older adults with mild to moderate hypertension: instead of regular table salt, participants used a mineral salt lower in sodium and higher in potassium and magnesium.
Over the study period, systolic blood pressure fell by about 8 mmHg and diastolic by about 3 mmHg. Importantly, participants didn’t overhaul their diets. The main change was the sodium–potassium–magnesium balance of the salt itself.
This study suggests that people often struggle with “sodium reduction” not because the physiology is wrong, but because adherence is hard. Shifting the mineral mix can sometimes achieve meaningful effects without demanding perfection elsewhere.
Potassium lowers blood pressure especially when sodium is high
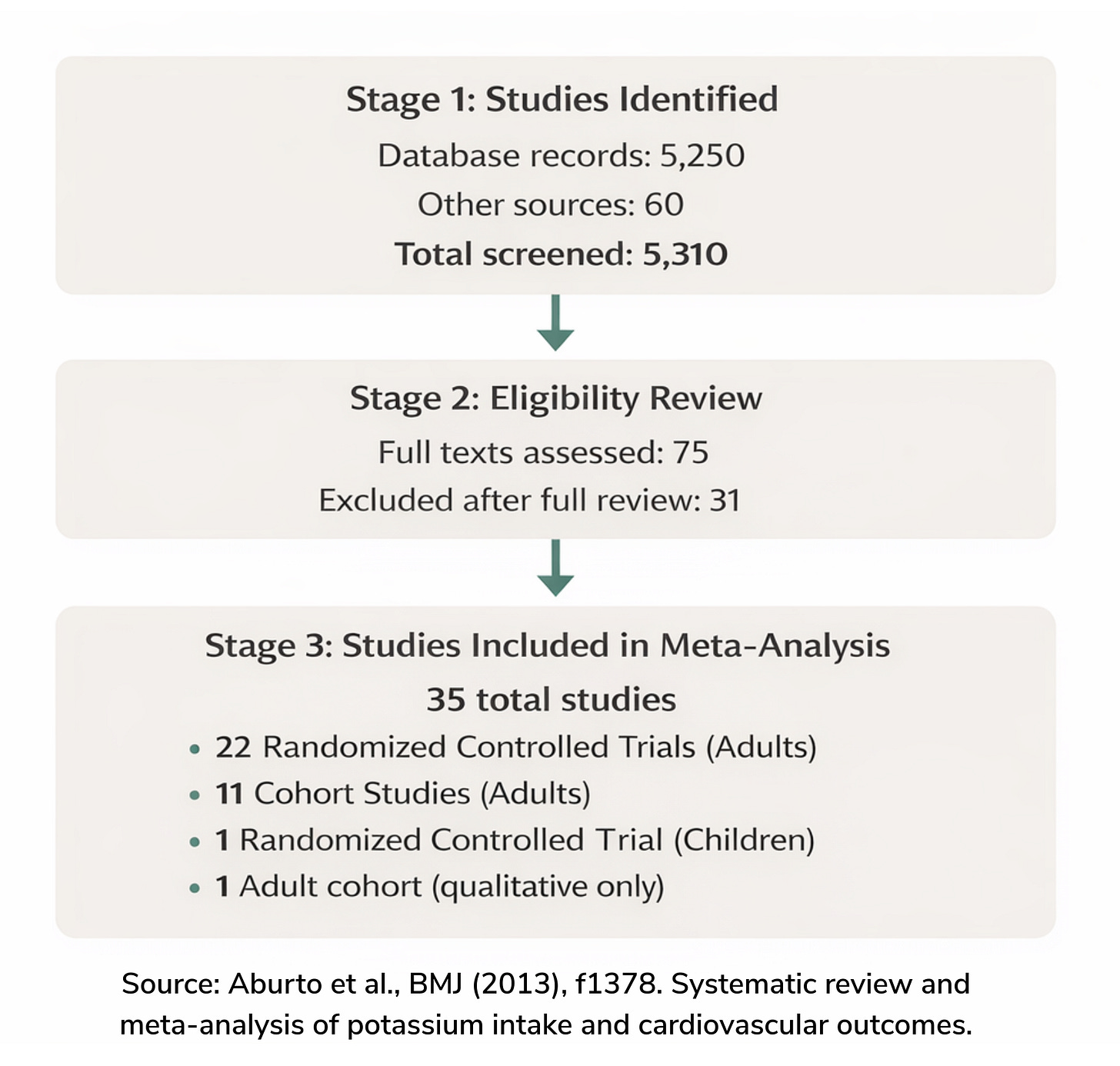
A large BMJ meta-analysis combined evidence from 22 randomized trials and 11 cohort studies to examine potassium intake and cardiovascular outcomes.
Higher potassium intake was associated with lower blood pressure, particularly in people with hypertension, and with a lower risk of stroke. Importantly, the review explored whether potassium’s effects varied depending on baseline sodium intake.
The conclusion was clear: potassium isn’t a standalone fix. Its benefits are strongest when sodium intake is high, highlighting that the ratio and balance between electrolytes matters more than any single number.
When potassium doesn’t work magnesium is often the missing piece
Clinical observations published in Archives of Internal Medicine revealed a problem doctors encounter regularly: potassium levels won’t correct if magnesium deficiency goes untreated.
Among patients with low potassium, 38–42% also had magnesium deficiency. Without restoring magnesium, potassium continued to be lost through the kidneys. The authors recommended that clinicians routinely check and treat magnesium when addressing hypokalemia.
This study explains why “just take potassium” sometimes fails. Magnesium acts as a gatekeeper, stabilizing potassium inside cells and reducing renal loss.
Blood pressure regulation isn’t driven by a single villain. It’s governed by an electrolyte system; sodium, potassium, and magnesium working together through the kidneys, blood vessels, and nervous system.
The evidence keeps pointing in the same direction:
lowering sodium helps, but lowering sodium while raising potassium and magnesium helps more. Diet patterns outperform isolated targets. And real physiology rewards balance over extremes.
Detailed Readings
Effect of increased potassium intake on cardiovascular risk factors and disease
Refractory Potassium Repletion A Consequence of Magnesium Deficiency